Emergency Guide to Rabies
If you have been bit by any animal you don’t know, domestic or wild, RUN don’t walk to an urgent care or emergency room. Call 811 and they can also direct you on your closest option.
Rabies has a 99.99% mortality rate, by the time you show symptoms you’re already dead. Dramatic? Sure, but also true.
Basic wound care is also important, because it’s not just rabies to worry about. Other blood and saliva borne diseases and infections can cut you down even if the bite “isn’t that serious,” this goes for scratches too that break the skin. Cat claws in particular can create huge problems even if they are indoor pets.
But we’re focusing on rabies: what is it, how is it prevented, how will you be treated?
What is Rabies?
Rabies is a saliva transmitted viral infection that can go from infected animals to humans. The virus attacks the nervous system and brain. Any mammal (warm-blooded animal) can be infected with the rabies virus.
Early symptoms of infection appear similar to flu symptoms:
- Chills
- Fever
- Excessive tiredness
- Headache
- Low/no appetite
- Insomnia
- Anxiety/irritability
- Aches and pains
- In some cases: tingling or numbness around bite
Prevention
Well first: don’t get bit. Yeah…rabies can’t be transmitted through contact with blood, urine, or feces of an infected animal. Still contact your doctor or call 811 if you are exposed to any of that because you can still be at risk for other parasites and diseases.
Secondly, vaccinate your pets. Just do it. If you don’t agree, stop reading here and let Murphy’s Law and Darwinism take you.
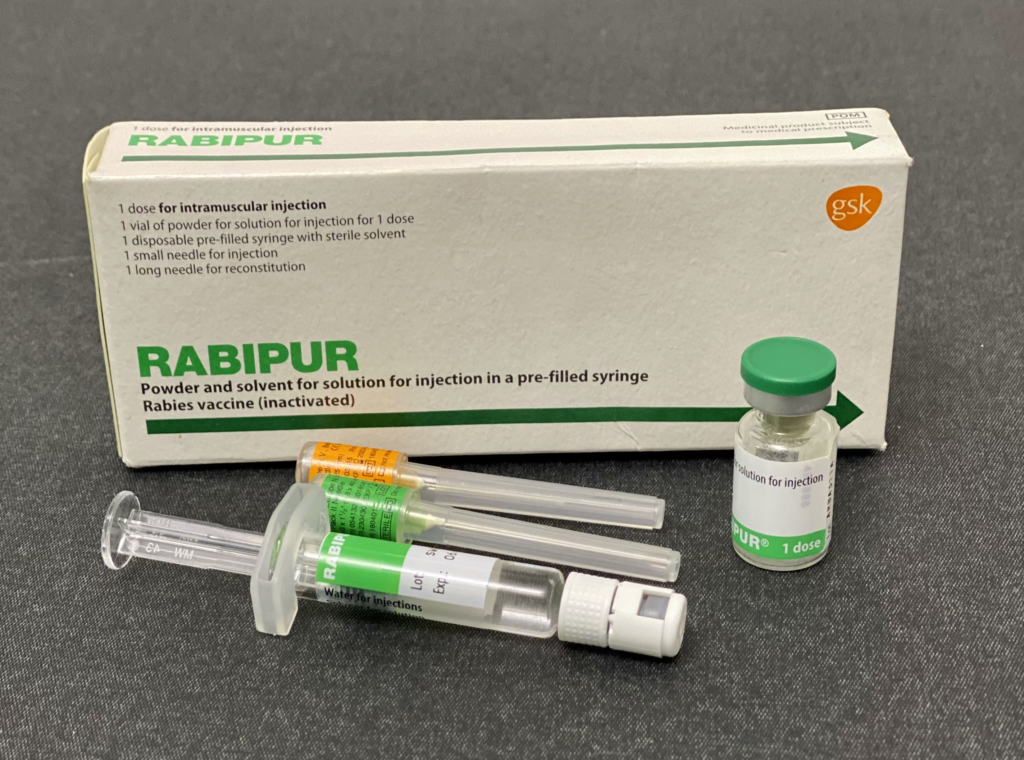
You can also vaccinate yourself if you know you’re going to be in a position where you could be exposed, be it work or leisure activities.
Treatment
Disclaimer: Please note that this is not medical advice to be taken above that of your service provider, EMS, etc. This information is to help you feel prepared in the case of injury, we make no claim to be medical professionals. Always call 911, 811, or your medical service provider in the case of illness or injury.
Immediately put pressure on the wound with a clean, dry cloth if it is deep enough to be bleeding freely. If someone is helping you make sure they have washed their hands with soap and water and are wearing clean latex or nitrile gloves.
If the wound is on the neck, head, face, hand, fingers, or feet call 811 or 911 immediately.
Wash the wound under warm running water with a mild soap (unscented if possible). Rinse the bite for 3 to 5 minutes under the water.
Apply an antibacterial ointment to the wound (remember not to put the tip of any tube onto the skin as this can contaminate the tube). Use the tip of a clean finger, cloth, or other applicator to take ointment and spread it on gently.
Put on a dry, sterile bandage and see a health care provider within 24 hours.
Once with a doctor, you will most likely be treated with the rabies vaccine: 5 shots over 14 days, thankfully this treatment is far less painful than it once was.
Like we said before, once you’re showing symptoms you’re screwed, which is why you head to medical care and say: “I’ve been bit by an animal.” Don’t take risks with your health and safety or that of others.
And please, for the love of all that is good and holy, get your pets vaccinated against rabies. No one needs Cujo in their neighborhood.
(Information from Mount Sinai, Alberta Health, Ontario fish and wildlife health, Government of Canada)
